The Peninsula
The Telemedicine Controversy in Korea

By Randall S. Jones
Covid-19 has had a profound economic and social impact in a number of areas, such as education and travel. Healthcare has also been affected, including a massive spike in the use of telemedicine, which was already used in a large majority of OECD countries, including Japan, as well as in China. However, Korea has not introduced telemedicine, even though it stands out as one of the world’s most wired nations. Telemedicine should be an important component of Korea’s New Deal. As President Moon said in May 2020, “the government will boldly execute the Korean New Deal so that Korea can lead new industries in the fields of digital and distance services”.
Telemedicine can be defined as the use of information and communication technology (ICT) to deliver healthcare at a distance. It allows healthcare, one of the most information-intensive sectors of the economy, to make greater use of information technology. Telemedicine is not limited to physicians; for example, nurse practitioners and clinical psychologists can also use it. Telemedicine includes two distinct aspects:
- Interactive or real-time telemedicine using direct and synchronous communication between providers and patients.
- Telemonitoring is the use of mobile devices and platforms to conduct routine medical tests and to communicate the results to healthcare workers. Data on patients, such as pulse, heart rate and blood glucose, can be collected remotely.
Potential benefits of telemedicine
There is growing evidence suggesting that healthcare delivered via telemedicine can be both safe and effective, resulting in better outcomes than conventional face-to-face care in some cases. Telemedicine can also be cost-effective. In a U.S. study, it was estimated that a typical visit to a doctor takes about two hours, including 37 minutes of travel. Of the 84 minutes at the clinic, only 20 minutes is face-to-face with a physician. The opportunity costs for the patient and the economy are very large. In addition, telemonitoring can be used for preventive care that can reduce the number of people requiring hospitalization.
Moreover, telemedicine enhances access to healthcare. Many people do not even make it to a doctor’s office due to various obstacles. In a study of 23 OECD countries, between 11% and 65% of people reported unmet medical needs in 2015-16 due to access barriers, such as waiting times, distance and transportation. Digital technologies thus have the potential to provide greater access to healthcare.
Korea, as a world leader in ICT, is well-positioned to benefit from telemedicine. Its ICT sector is a driver of innovation, and has high shares of value added and employment. Business sector R&D in ICT is high, resulting in more ICT-related patents (as a percentage of total IP5 patent families) than any other OECD country. Korea also outperforms many OECD countries in fixed and mobile broadband networks with very high penetration of fiber in fixed networks and well-developed mobile broadband.
The potential benefits of telemedicine are particularly large in Korea for a number of reasons:
- Korea faces the most rapid population aging among OECD countries, which will sharply increase healthcare spending. Indeed, the old-age dependency ratio (the ratio of the population aged 65 and over to the population aged 15-64) is currently the sixth lowest among the 37 OECD countries but is projected to be the highest by 2060. Policies, including telemedicine, are essential to enhance the efficiency of healthcare.
- About a quarter of Korea’s elderly population lives in rural areas. Telemedicine would increase access to healthcare for those who need it most.
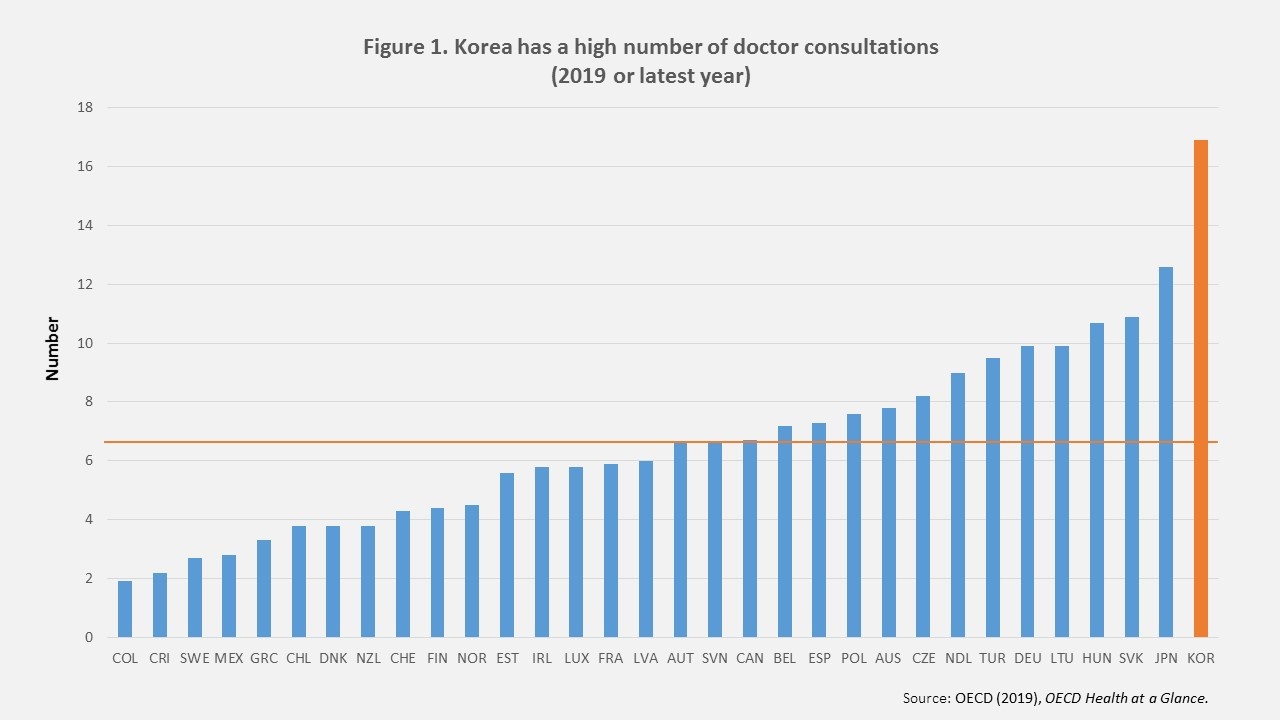
- The number of doctor consultations per capita in Korea was 16.6 in 2018, the highest in the OECD and more than double the average of 7.6 (Figure 1). Replacing some of the in-person visits with virtual consultations would result in large reductions in travel and waiting times.
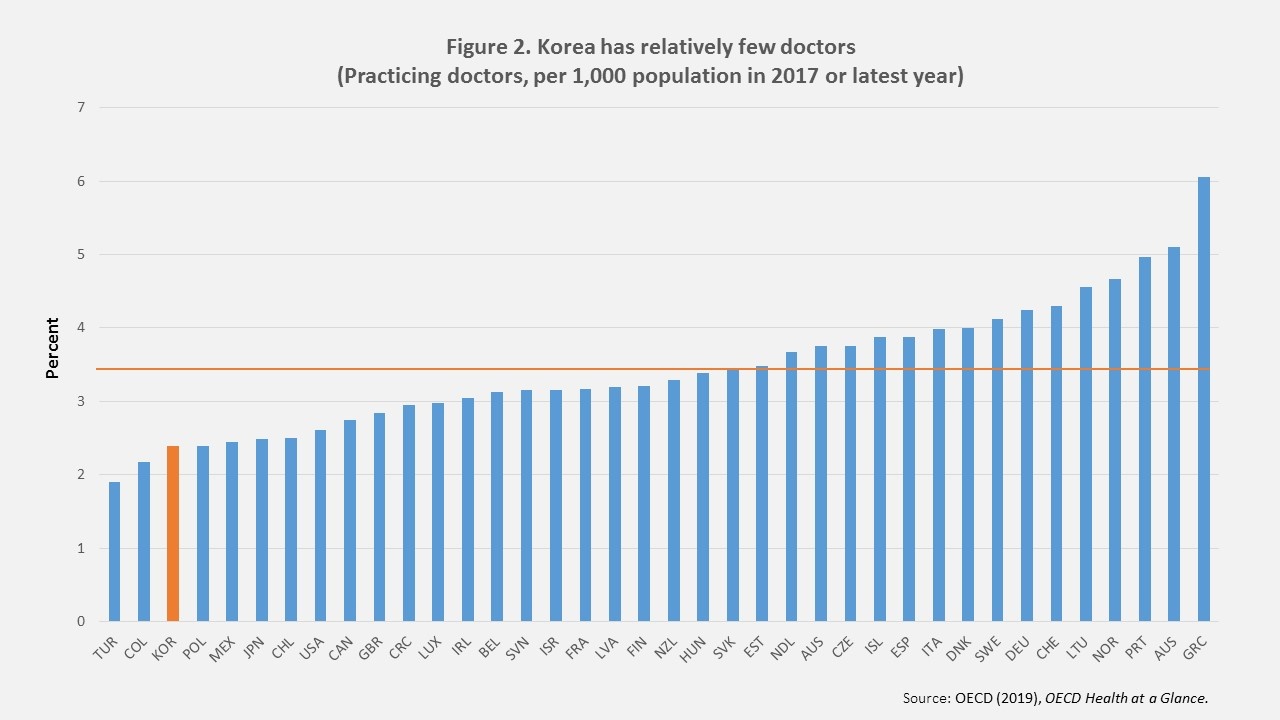
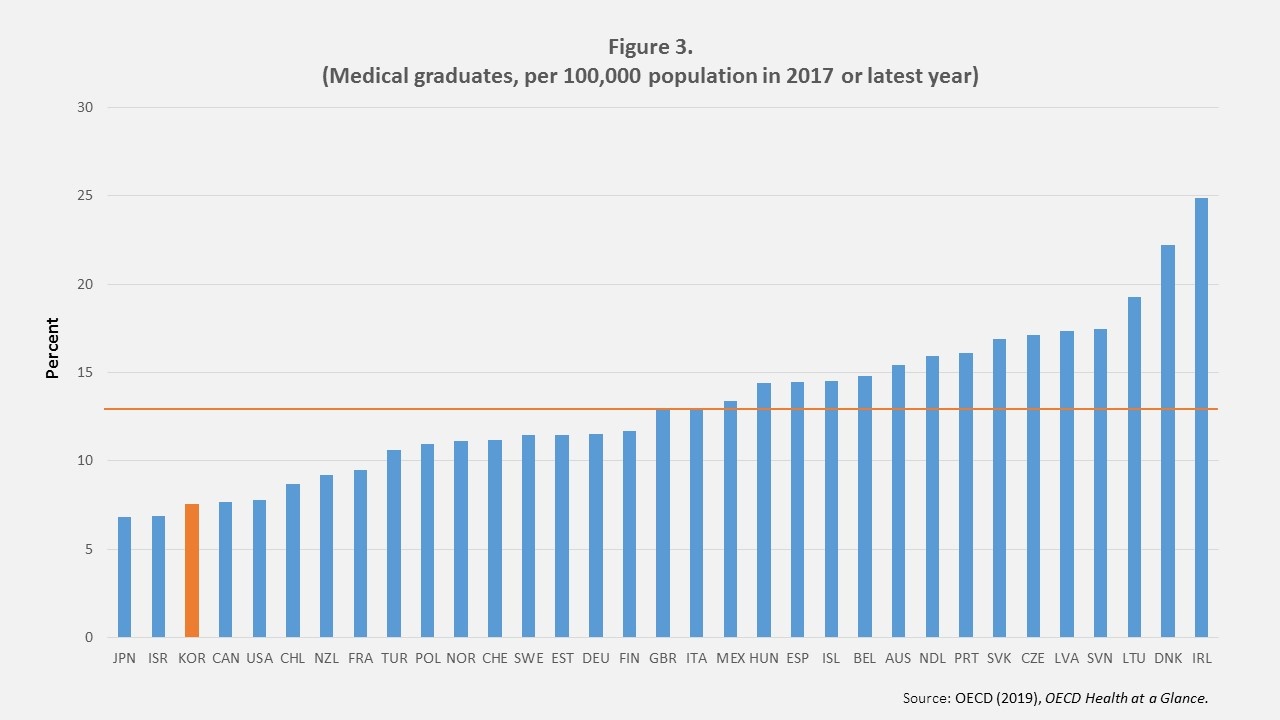
- Korea only has 2.3 doctors per 1,000 population in 2017, the third lowest among OECD countries after Turkey and Columbia (Figure 2). That is likely to remain the case as the number of medical school graduates in 2017 was also the third lowest in the OECD (Panel B). The relatively small number of doctors risks leaving some parts of the country with inadequate healthcare, increasing the need for telemedicine. In addition, the greater flexibility of telemedicine could allow better use of doctors’ time.
The coronavirus pandemic has expanded the use of telemedicine in many countries. In Korea, the government has allowed doctors to offer medical services to patients via telephone on a temporary and limited basis since February 2020. Between February 24 and May 31, about 360,000 telemedicine bills were issued by 4,651 hospitals, according to government data. Telemedicine has thus played a useful role in providing treatment while protecting medical staff from being exposed to the virus. Telemedicine will also help prepare for a possible second wave of coronavirus infections. Few cases of misdiagnosis or other problems in the telemedicine consultations have been reported. In addition, a regulatory change introduced on June 25th will allow certain hospitals to provide remote medical services to overseas Korean amid the coronavirus pandemic beginning in September. This exemption will last for two years.
Significant opposition to the introduction of telemedicine in Korea
With the National Assembly beginning its four-year term in May 2020, the government is now discussing the possible introduction of a bill to revise Korea’s Medical Act to allow telemedicine. Yong-beom Kim, Vice Minister of Economy and Finance, said that the Ministry “is sticking to its stance that there is a need to actively review the implementation of telemedicine services”.
However, it continues to face significant opposition from the Korea Medical Association (KMA), which represents some 130,000 physicians, and civic organizations. After the introduction of legislation in 2014 to allow telemedicine, the KMA threatened to strike. Moreover, its cooperation with pilot projects to assess the feasibility of telemedicine has been limited. In 2019, the ruling Democratic Party drafted a bill that called for providing telemedicine services to people on remote islands, prison inmates, deep-sea fishermen and soldiers deployed to hard-to-reach areas, but the bill was not submitted due to strong opposition.
Dae-zip Choi, president of the KMA, said that “We have no choice but to wage an extreme battle if the government pushes for telemedicine because it could undermine the nation’s medical system”. The opposition reflects a number of concerns. First, telemedicine could lead to misdiagnoses and the theft of personal data. Second, it could hurt smaller clinics, which rely on close geographical proximity to their patients and do not have the resources to invest in telemedicine. If telemedicine were allowed, such clinics could be replaced by doctors associated with large, well-known hospitals. The collapse of small clinics would ultimately reduce access for essential in-person healthcare. Third, opponents fear that telemedicine will create a lucrative market for “smart” health technologies that will benefit only those who can afford them. Fourth, there is concern that allowing telemedicine would open the way for for-profit hospitals. Under the Medical Service Act, for-profit hospitals are prohibited.
Conclusion
Telemedicine has the potential to expand access to healthcare, which will help cope with the immediate threat of COVID-19 and improve health outcomes in the long run. Moreover, it can enhance the efficiency of healthcare, helping contain the rise in healthcare spending as the population ages. At the same time, telemedicine may introduce new risks. The guiding principle should be to focus on telemedicine services that improve healthcare quality and provide clear benefits to patients. In sum, telemedicine can help improve equity and efficiency in healthcare, while contributing to the government’s goal of making Korea a “digital powerhouse”.
Randall Jones is a Visiting Fellow at Columbia University and a Non-Resident Fellow at the Korea Economic Institute of America. The views expressed here are the author’s alone.
Graphics by Juni Kim, Senior Manager for Operations and Technology, Korea Economic Institute of America.
Photo from ITU Pictures’ photostream on flickr Creative Commons.
